1. "A 28 year female comes to the emergency room complaining of 6 days of fevers with shaking chills. Over the past 2 days, she has also developed a productive cough with greenish sputum, which occasionally is blood streaked. She reports no dyspnea, but sometimes experiences chest pain on deep inspiration.
She denies headache, abdominal pain, urinary symptoms, vomiting, or diarrhea. She smokes cigarettes and marijuana regularly, drinks beers daily, but denis IV drug use.
On exam, her temperature is 102.5 F, heart rate is 109 bpm, bp 128/76 mmHg, and resp rate at 23 breaths per minute. She is alert and talkative. She has no oral lesions, and funduscopic exam reveals no abnormalities. She is tachycardic, but regular with a harsh holosystolic murmur at the left lower sternal border that increases with inspiration. Chest examination revels inspiratory rales bilaterally.
a. What is your clinical suspicion at this point using your clinical gestalt?
Suspected Endocarditis (S. aureus)
Labs:
WBC 17,500/mm3 (Diff: 84% PMN's, 7%bands, 9% lymphs)
Hemoglobin 14 g/dL
Hematocrit 42%
Platelet 189,000/mm3
Liver function and urinalysis are normal
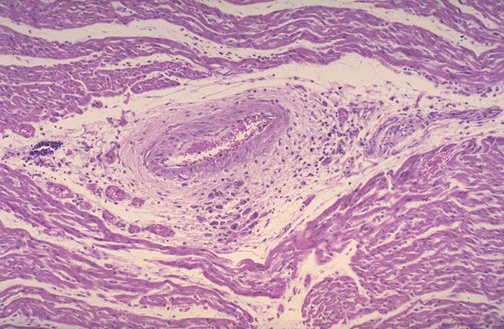
b. What general process are you concerned about after seeing the lab results? Use the following picture. Describe what you can appreciate.
Infection;
Microscopically, the valve in infective endocarditis demonstrates friable vegetations of fibrin and platelets (pink) mixed with inflammatory cells and bacterial colonies (blue). The friability explains how portions of the vegetation can break off and embolize.
c. Identify all 4 of the following clinical presentations. Identify the ONE of the four that matches the history of this patient.
Clinical Presentation 1- ROTH SPOTS
-Funduscopic examination
Clinical Presentation 2- TRACK MARKS
-On both of her forearms, you notice this...though you don't notice erythema, warmth, or tenderness.
Clinical Presentation 3-Janeway Lesions
-Non-tender, small erythematous or hemorrhagic macular or nodular lesions on the palms or soles only a few millimeters in diameter
Clinical Presentation 4-OSLERS NODES
-Painful, red, raised lesions found on the hands and feet.
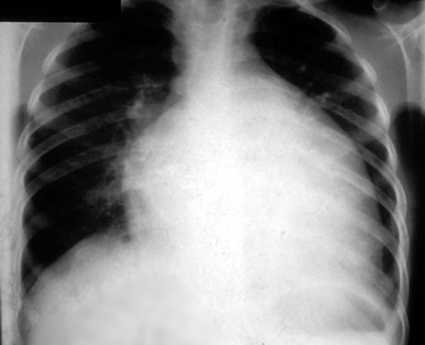
You decide to get a chest radiograph which shows the following:
The radiologist describes them as multiple peripheral, ill-defined nodules, with some cavitation.
d. What is your diagnosis and next step?
Septic Pulmonary Emboli
Obtain serial blood cultures and institute broad spectrum antibiotics. Most likely S. aureus...so treat with Vancomycin.